THE ARCHIVES
A collection of past ISSCR events, historical documents, and award winners.
For more information on historical events, meetings, and programs, please contact us at isscr@isscr.org

ISSCR 2025 Annual Meeting | Hong Kong
The global stem cell community gathered for a week of standout science, discovery, and networking at the ISSCR 2025 Annual Meeting. With over 2,500 members joining us from around the world, we were able to effectively connect and share our wide array of thoughts, research, and perspectives through this event.
Through hundreds of talks and presentations, scientists revealed breakthroughs in stem cell science and applications to human health. Whether you joined for one of our Plenary Sessions highlighting award winners and standout science in the field or joined one of our Special Sessions, your input and participation helped make the meeting a success.













































For more than 20 years the International Society for Stem Cell Research has convened global leaders and the next generation of scientists for the ISSCR Annual Meeting. The conference sets a precedent for global collaboration, encourages excellence and rigor, and shines a bright light on regions of the world excelling in research and clinical applications.
Past ISSCR Annual Meetings

2025 ISSCR PSC-Derived Therapies International Symposium
Boston, USA | 11-12 December 2025
Stem cell scientists, researchers, and clinicians came together on 11-12 December 2025 in Boston, USA to share the latest research and clinical applications for pluripotent stem cell-derived therapies.





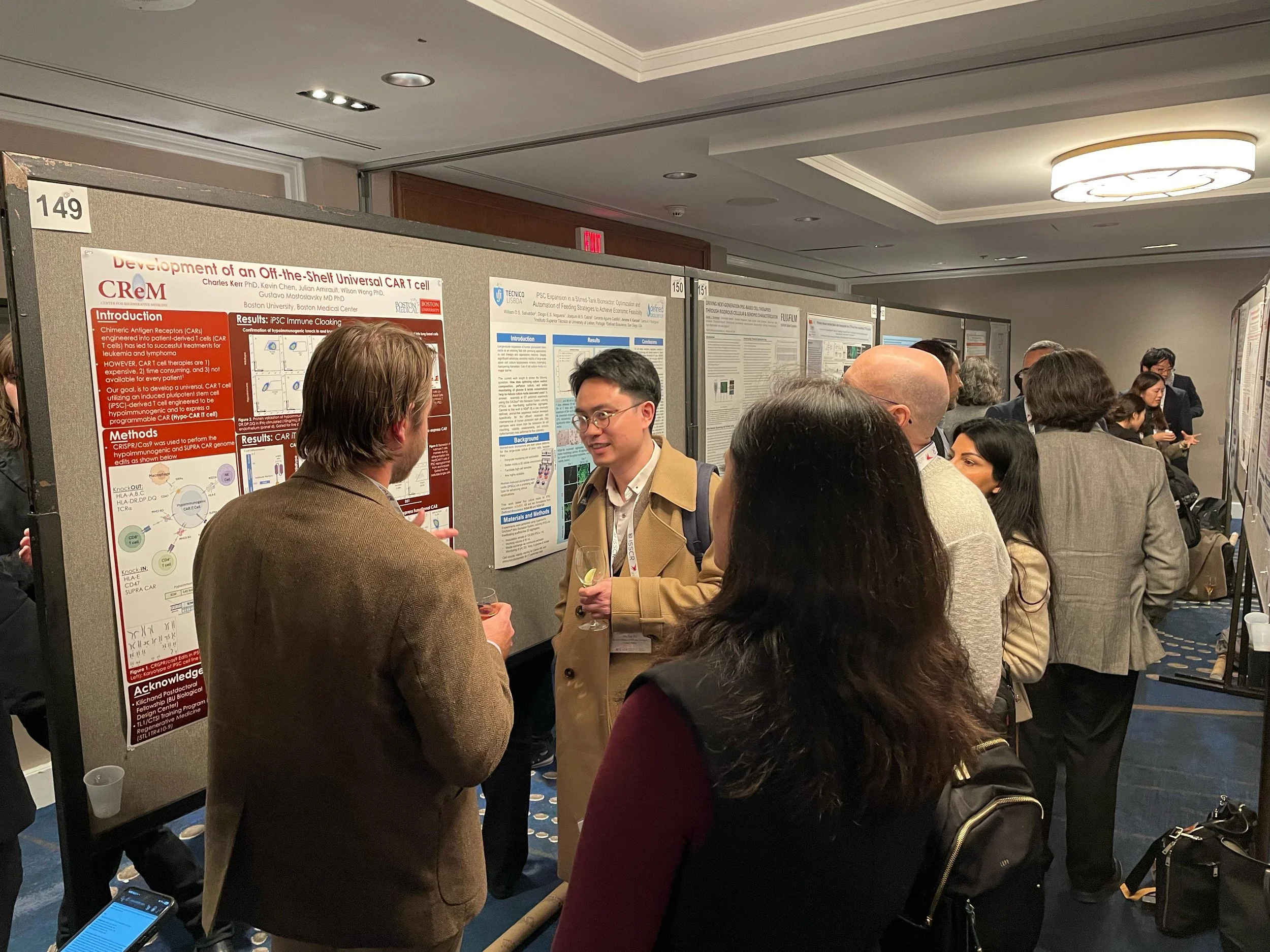










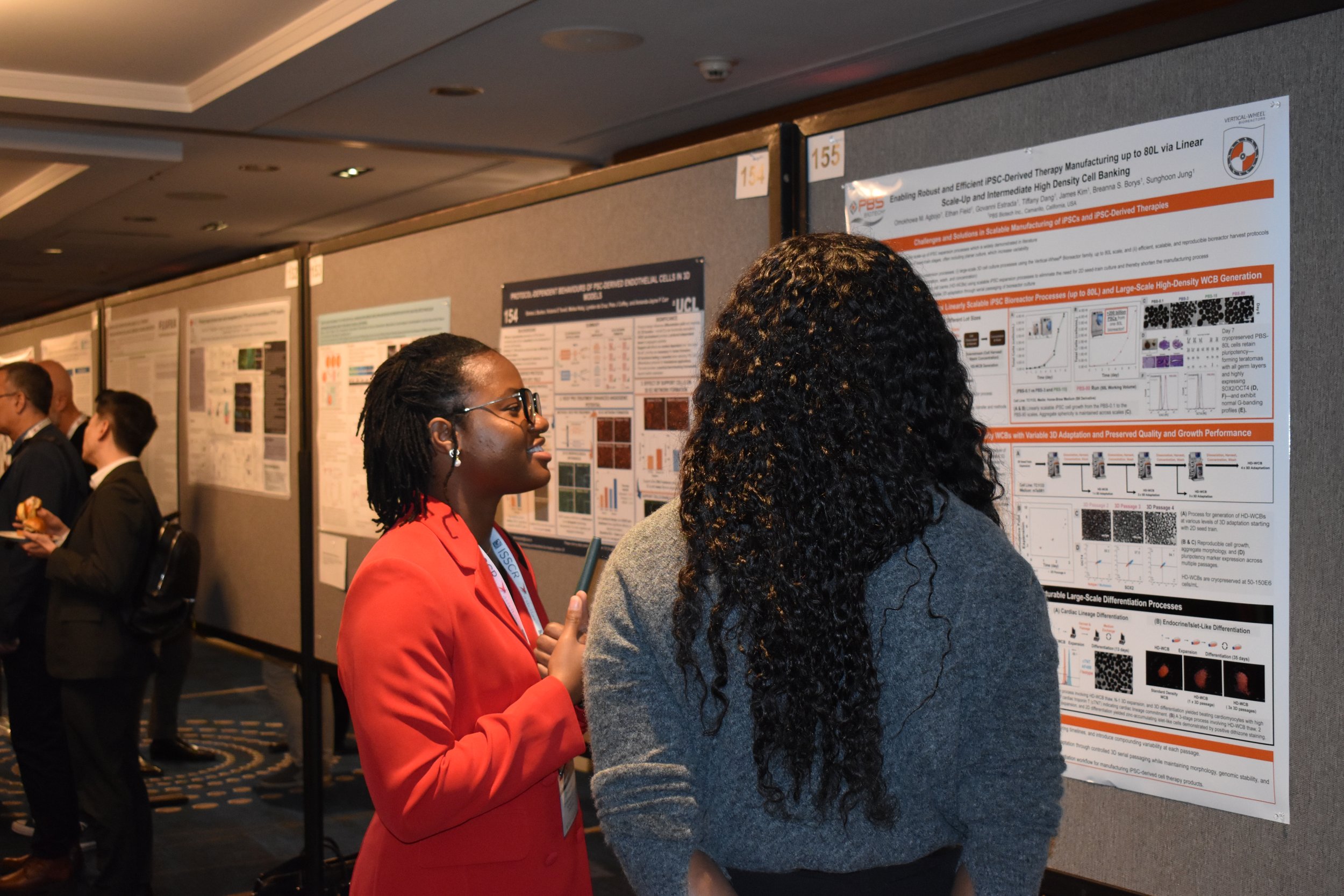
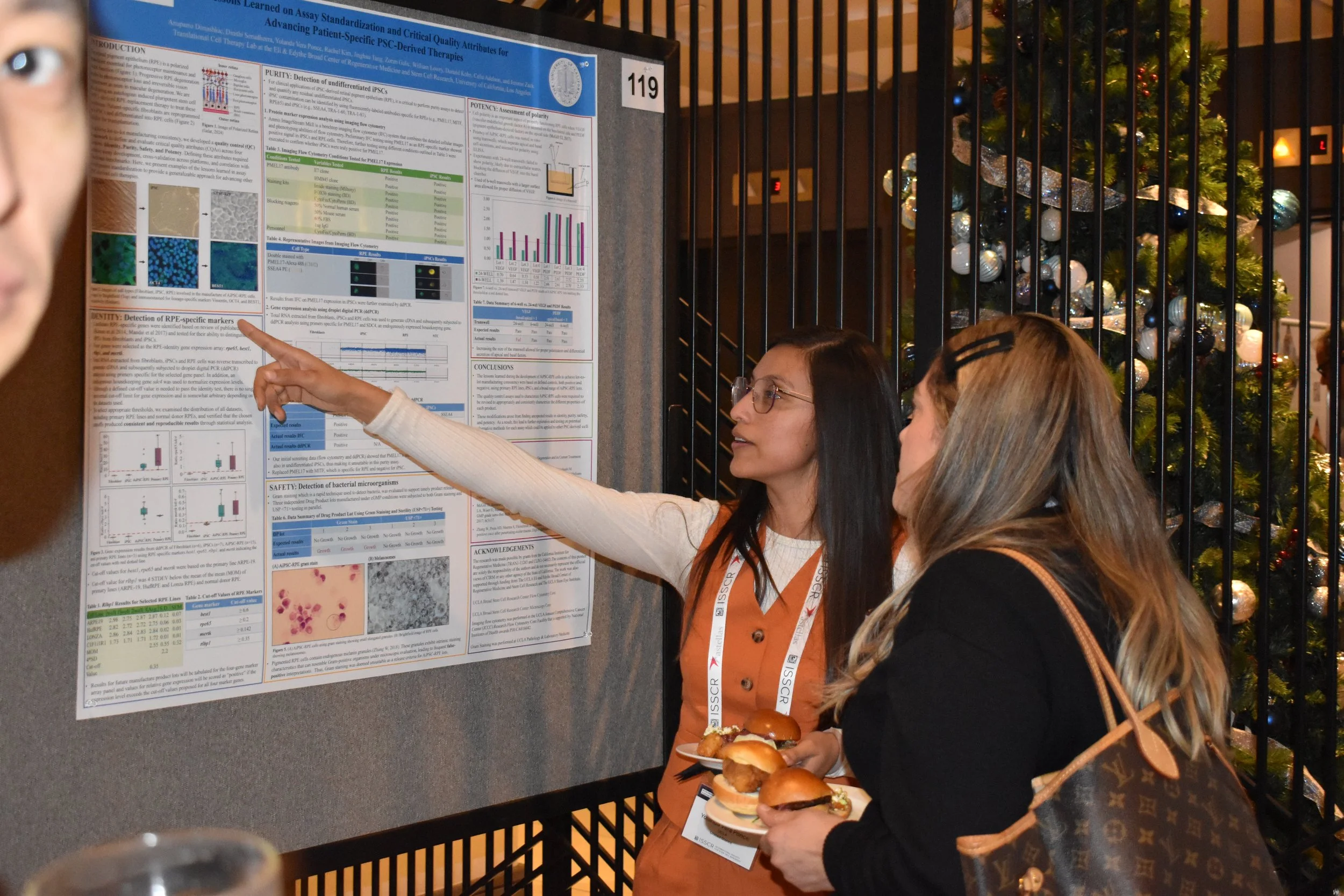



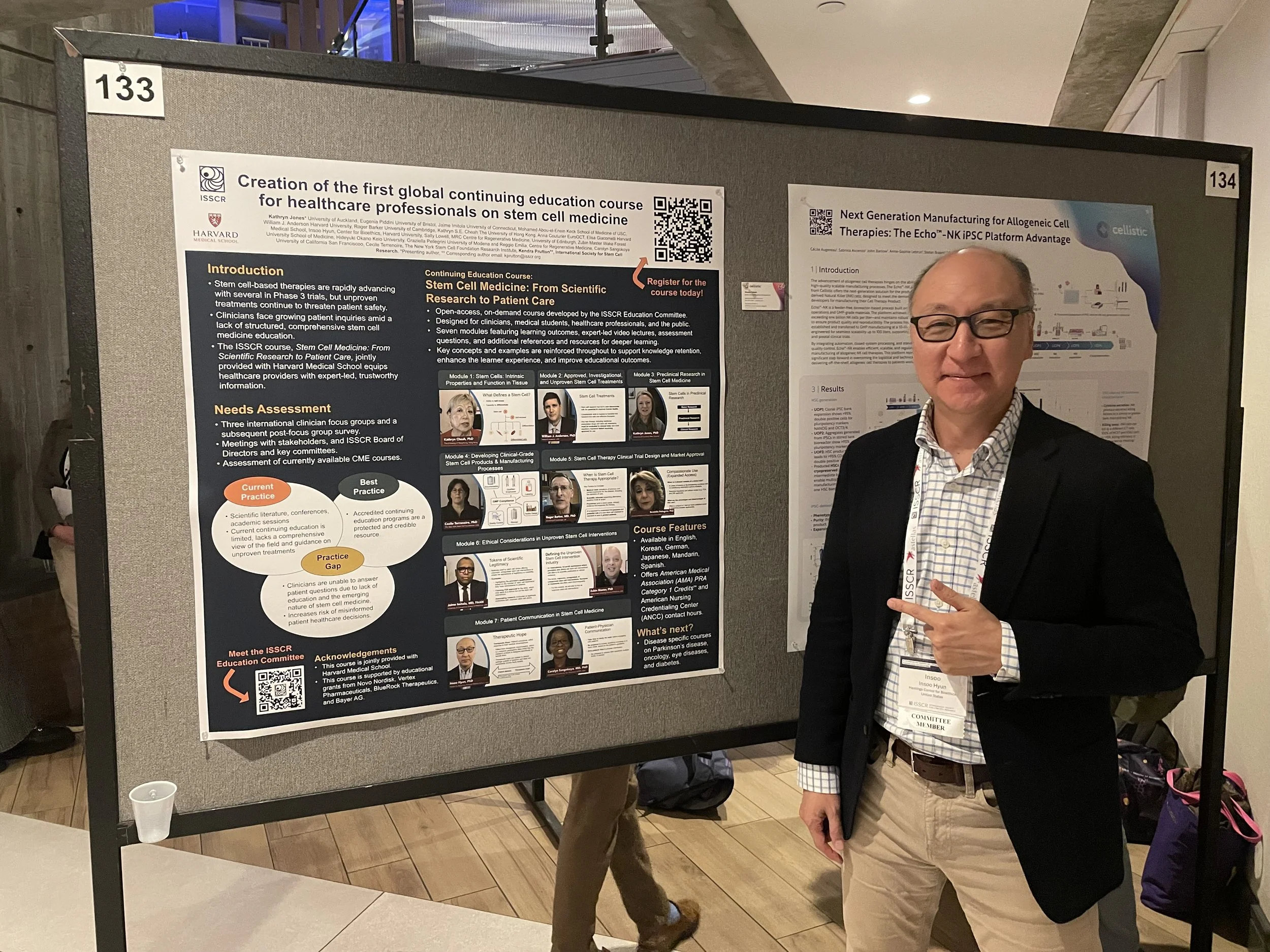
Congratulations to the PSC-Derived Therapies International Symposium Poster Award Winners
David Li
University of Toronto, Canada
Marc Estarellas
University of Barcelona, Spain
Austin Feeney
University of Wisconsin-Madison, USA
Charles Kerr
Boston University, USA
Thank You to the Poster Award Sponsor:

The ISSCR International Symposia were designed to be smaller, more intimate meetings that bring together the world's leading experts in a specific area of stem cell science and/or application to share their research, build relationships and collaborations and move the field forward.
Hosted in state-of-the-art venues across the globe, the program often highlights regional accomplishments by partnering with the host country or region's stem cell organizations and industry partners.
Past ISSCR International Symposia

View past digital webinars, events, and programs on
the ISSCR Member Library.
Key Topics from the 2021 Guidelines
-
This page assembles the sections of the Guidelines that specifically address research involving the culture of human embryos. Other sections of the Guidelines may be relevant to such research (e.g., Section 2.1 Review Process, Section 2.3 Procurement and Informed Consent of Human Biological Materials, and Section 2.4 Derivation, Banking, and Distribution of Human Cell Lines).
2.2.2 Category 2
2.2.2 Category 2. Forms of research with embryos, certain chimeras, and stem cell-based embryo models that are permissible only after review and approval through a specialized scientific and ethics review process. A comprehensive review should be coordinated with other relevant oversight, such as that provided by human subjects review committees, in vitro fertilization (IVF) clinic oversight bodies, and animal research review processes (see 2.2.1), and the research should comply with local law and policy. All such research should have a compelling scientific rationale and necessitate the use of these materials rather than employ alternative models. The research should use the minimum number of embryos necessary to achieve the scientific objective. Forms of research requiring comprehensive review by a specialized review process encompass the following activities:
Procurement and use of IVF human embryos for research in vitro.
Procurement of human gametes to create research embryos in vitro.
Research that generates human gametes from any progenitor cell type in vitro, when this entails performing studies of fertilization that produce human zygotes and embryos. The gametes may be derived from human pluripotent stem cells, oogonia, or spermatogonial stem cells that have been maintained in vitro, and they may be genetically modified or not. Any human embryos obtained from such gametes must only be studied in vitro, or be used to derive stem cell lines, such as embryonic stem cells.
Research involving the genetic alteration of human embryos or gametes used to make embryos in vitro.
Derivation of new cell lines from human embryos (not confined to pluripotent cell lines).
Research involving the in vitro culture of human embryos where embryos are maintained in culture until the formation of the primitive streak or 14 days from fertilization, whichever occurs first.
Culture of Human Embryos Beyond formation of the primitive streak or 14 Days
It is currently not technically feasible to culture human embryos beyond formation of a primitive streak or 14 days post-fertilization. However, culture systems are evolving, making this a possibility in the near future. Understanding the primitive streak, early germ layer development and primordial germ cell formation in humans is crucial to improve our understanding of and interventions for infertility, in vitro fertilization, pregnancy loss, and developmental disorders that occur or originate soon after implantation. Research using embryos is also crucial to validate integrated stem cell-based embryo models, which in the future may provide a more practical alternative to understanding some aspects of early human development.
Recommendation 2.2.2.1: Given advancements in human embryo culture, and the potential for such research to yield beneficial knowledge that promotes human health and well-being, the ISSCR calls for national academies of science, academic societies, funders, and regulators to lead public conversations touching on the scientific significance as well as the societal and ethical issues raised by allowing such research. Should broad public support be achieved within a jurisdiction, and if local policies and regulations permit, a specialized scientific and ethical oversight process could weigh whether the scientific objectives necessitate and justify the time in culture beyond 14 days, ensuring that only a minimal number of embryos are used to achieve the research objectives.
-
This page assembles the sections of the Guidelines that specifically address research involving stem cell-based embryo models. Other sections of the Guidelines may be relevant to such research (e.g., Section 2.1 Review Process, Section 2.3 Procurement and Informed Consent of Human Biological Materials, and Section 4. Communications).
2.2.1 Category 1
2.2.1A Category 1A. Research determined to be exempt from a specialized scientific and ethics oversight process after being assessed by the appropriate existing mandates and committees for laboratory research. Category 1A research includes the following activities:
Research on stem cell culture systems that model specific stages of development or specific anatomic structures rather than the continuous development of an intact embryo or fetus. These would include but are not restricted to models of amnion formation, neural tube development, development of primordial germ cells, placental structures, 2D or 3D models of gastrulation or post-gastrulation events, and in vitro stem cell-derived organoids in culture that recapitulate most aspects of organ function, but not those that fall under subsequent categories.
2.2.1B: Category 1B. Research that is reportable to the entity or body responsible for the specialized scientific and ethics oversight process, but not normally subject to further or ongoing review, at the discretion of the entity responsible for the oversight process and subject to regulations and policies in the jurisdiction. Category 1B research includes the following activities:
Research that entails the in vitro formation of human stem cell-based embryo models that are not intended to represent the integrated development of the entire embryo including its extraembryonic membranes.
Scientists pursuing Category 1A and B research are recommended to consult with appropriate institutional review committees or the committee or body responsible for the specialized scientific and ethics review process (see Recommendation 2.1.3) to determine the categorization of new research proposals. Committees with the jurisdiction over the relevant research should oversee the provenance of cells, tissues and derived human pluripotent stem cell lines to ensure that procurement and derivation is deemed acceptable according to the principles outlined in this document (see section 2.3.5) and is in compliance with rigorous scientific, legal, and ethical standards.
2.2.2 Category 2
2.2.2 Category 2. Forms of research with embryos, certain chimeras, and stem cell-based embryo models that are permissible only after review and approval through a specialized scientific and ethics review process. A comprehensive review should be coordinated with other relevant oversight, such as that provided by human subjects review committees, in vitro fertilization (IVF) clinic oversight bodies, and animal research review processes (see 2.2.1), and the research should comply with local law and policy. All such research should have a compelling scientific rationale and necessitate the use of these materials rather than employ alternative models. The research should use the minimum number of embryos necessary to achieve the scientific objective. Forms of research requiring comprehensive review by a specialized review process encompass the following activities:
Generation of stem cell-based embryo models that represent the integrated development of the entire embryo including its extraembryonic membranes. These integrated stem cell-based embryo models should be maintained in culture for the minimum time necessary to achieve the scientific objective.
2.2.3 Category 3
2.2.3B Category 3B: Prohibited research activities. Research under this category should not be pursued because of broad international consensus that such experiments lack a compelling scientific rationale or are widely considered to be unethical. Such research includes:
Transfer of human stem cell-based embryo models to the uterus of either a human or animal host.
Public Representation of Science
Recommendation 4.1: The stem cell research community should promote accurate, current, balanced, and responsive public representations of stem cell research.
The high level of public and media interest in the field provides stem cell scientists with ample opportunities to communicate their findings through a variety of popular and social media channels. The research community is encouraged to responsibly engage interactively with the public through outreach and communications and by providing opportunities for public comment and feedback on scientific advances.
While such opportunities may allow scientists to gain recognition and understanding for their work among non-specialists, they also have the potential to fuel inaccurate public perceptions about the current state of scientific progress, potential for application, and associated risks and uncertainties (Kamenova and Caulfield, 2015). Scientists, clinicians, bioethicists, science communications professionals at academic and research institutions, and industry spokespersons should strive to ensure that benefits, risks, and uncertainties of stem cell science are not understated, misrepresented or overstated (see Recommendation 3.3.4.1). Additionally, due to public interest and concern in the ethics of human pluripotent stem cell research, and in order to ensure complete transparency of research and translational activities, the origin of stem cell materials should be clearly specified in all communications.
Care should be exercised throughout the science communication process, including in the promotion of research and translation activities, as well as in the presentation of scientific results, the use of social media, and in any communication with print and broadcast media. Particular caution should be exercised when preparing press releases and other types of promotional material. Researchers should make efforts to seek timely corrections of inaccurate or misleading public representations of research projects, achievements, or goals. Scientists should also be particularly careful about disclosing research findings that have not passed peer review, as premature reporting can undermine public confidence if findings are subsequently disproven. For example, if researchers post online preprints that have not been peer-reviewed, readers should be informed of the preliminary nature of such manuscripts.
Researchers must unintentionally avoid and correct inaccurate misconceptions in any communications regarding chimeras, genome editing, and other issues with a long history in the public imagination. While organoids, chimeras, embryo models, and other stem cell-based models are useful research tools offering possibilities for further scientific progress, limitations on the current state of scientific knowledge and regulatory constraints must be clearly explained in any communications with the public or media. Suggestions that any of the current in vitro models can recapitulate an intact embryo, human sentience or integrated brain function are unfounded overstatements that should be avoided and contradicted with more precise characterizations of current understanding. This is particularly relevant to brain organoids and human-animal chimeras, where any statements implying human cognitive abilities, human consciousness or self-awareness, as well as phrases or graphical representations suggesting human-like cognitive abilities risks misleading the public and sowing doubts about the legitimate nature of such research. Likewise, forward-looking statements on inherently uncertain developments, such as predictions on time required until clinical application, the likelihood of product approval, or speculation on the potential economic impact of currently unrealized technologies, must be accurate, circumspect, and restrained.
The stem cell community should work closely with communications professionals at their institution to create information resources that are easy to understand without oversimplifying, and that do not underplay risks and uncertainties or exaggerate potential benefits. Similarly, research-sponsoring institutions and communications professionals have a responsibility to ensure that any informational materials referring to research achievements adhere to these principles. Additionally, the scientists in charge of the research findings that are featured in informational materials should review and agree to the content prior to release. For potentially sensitive or high-profile cases, it is advisable to seek additional comments from independent experts to ensure objectivity and balance, place research in context of existing body of evidence, and help identify study limitations and alternative interpretations of key findings.
Glossary
Stem cell-based embryo models: Advances in cellular engineering make possible the assembly, differentiation, aggregation, or re-association of cell populations in a manner that models or recapitulates key stages of embryonic development. Such experimental systems can provide essential insights into embryo and tissue development but raise concerns when such structures achieve complexity to the point where they might realistically manifest the ability to undergo further integrated development if cultured for additional time in vitro. There are two types of stem cell-based embryo models.
Non-integrated stem cell-based embryo models: These stem cell-based embryo models will experimentally recapitulate some, but not all aspects of the peri-implantation embryo, for example differentiation of the embryonic sac or embryonic disc in the absence of extraembryonic cells. These stem cell-based embryo models do not have any reasonable expectations of specifying additional cell types that would result in formation of an integrated embryo model. Gastruloids are an example of a non-integrated stem cell-based embryo model.
Integrated stem cell-based embryo models: These stem cell-based embryo models contain the relevant embryonic and extra-embryonic structures and could potentially achieve the complexity where they might realistically manifest the ability to undergo further integrated development if cultured for additional time in vitro. Integrated stem cell-based embryo models could be generated from a single source of cells, for example expanded potential human pluripotent stem cells capable of coordinately differentiating into embryonic and extraembryonic structures. Alternatively, integrated stem cell-based embryo models could also be generated through the formation of cellular aggregates where extraembryonic/embryonic cells from one source are combined with embryonic/extraembryonic cells from different sources to achieve integrated human development. This might include using non-human primate cells as one of the sources. Previous restrictions on preimplantation human embryo culture (the “14-day/primitive streak rule”) were not written to apply to integrated stem cell-based embryo models. Thus, these guidelines specify the imperative for specialized review when such research is designed to model the integrated development of the entire embryo including its extraembryonic membranes. A guiding principle of review should be that the integrated stem cell-based embryo models should be used to address a scientific question deemed highly meritorious by a rigorous review process. Blastoids are an example of an integrated stem cell model.
-
This page assembles the sections of the Guidelines that specifically address research involving the transfer of human stem cells into animals. Other sections of the Guidelines may be relevant to such research (e.g., Section 2.1 Review Process and Section 2.3 Procurement and Informed Consent of Human Biological Materials).
2.2.1 Category 1
2.2.1A: Category 1A. Research determined to be exempt from a specialized scientific and ethics oversight process after being assessed by the appropriate existing mandates and committees for laboratory research. Category 1A research includes the following activities:
The transplantation of human stem cells, their derivatives, or other human cells into postnatal animal hosts (see Recommendation 2.2.1.1).
2.2.1B: Category 1B. Research that is reportable to the entity or body responsible for the specialized scientific and ethics oversight process, but not normally subject to further or ongoing review, at the discretion of the entity responsible for the oversight process and subject to regulations and policies in the jurisdiction. Category 1B research includes the following activities:
Chimeric embryo research in which human pluripotent stem cells are transferred into non-human, mammalian embryos and cultured in vitro for the minimum time necessary to achieve the scientific objective without gestation.
Scientists pursuing Category 1A and B research are recommended to consult with appropriate institutional review committees or the committee or body responsible for the specialized scientific and ethics review process (see Recommendation 2.1.3) to determine the categorization of new research proposals. Committees with the jurisdiction over the relevant research should oversee the provenance of cells, tissues and derived human pluripotent stem cell lines to ensure that procurement and derivation is deemed acceptable according to the principles outlined in this document (see section 2.3.5) and is in compliance with rigorous scientific, legal, and ethical standards.
Category 1B covers in vitro chimeric embryo research and in vitro gametogenesis for which there is no intent to generate a human embryo or fetus. Researchers are encouraged when possible to report on existing or planned in vitro experiments to the committee responsible for the specialized scientific and ethics oversight process to help identify cases that may warrant full review in the future.
Studies Transplanting Human Stem Cells or Their Direct Derivatives into the Central Nervous Systems of Animals
Recommendation 2.2.1.1: Research involving the transfer of human stem cells or their direct neural and/or glial derivatives into the central nervous systems of postnatal animal hosts requires review by institutional animal research oversight committees supplemented by reviewer expertise in stem cell or developmental biology. (ISSCR Guidelines, 2006; Academy of Medical Sciences, 2011). Such oversight should weigh the potential benefits of the research and should utilize available baseline non-human animal data grounded in rigorous scientific knowledge or reasonable inferences and involve a diligent application of animal welfare principles.
Institutions should determine whether research involving human cells that have the capacity to integrate into the nervous systems of laboratory animals requires supplementation of the pre-existing animal research review process with scientists and ethicists that have relevant topic-specific expertise.
To assist review and oversight of stem cell-based human-to-non-human animal research, the ISSCR has provided an advisory report that guides reviewers through a series of considerations not typically covered by institutional animal research committees, but that are relevant for review (Hyun et al., 2021). Past experiences with genetically altered laboratory animals have shown that reasonable caution might be warranted if changes carry the potential to produce new defects and deficits. Current best practices dictate that research involving modified animals must involve the following:
the establishment of baseline animal data;
ongoing data collection during research concerning any deviation from the norms of species-typical animals;
the use of small pilot studies to ascertain any changes in the welfare of modified animals; and
ongoing monitoring and reporting to animal research oversight committees authorized to decide the need for real-time changes in protocols and, if necessary, the withdrawal of animal subjects.
Research that may result in the presence of human gametes and their precursors in the gonads of laboratory animals is of not of significant ethical concern per se, as long as the animals are not allowed to breed (see Category 3 below).
Reviewers and investigators should follow the proposed ethical standards presented in the 2020 white paper and Appendix 1, while exercising appropriate judgment in individual situations. Research involving animals should also generally comply with the principles of the 3Rs (see: www.nc3rs.org.uk) and follow the ‘ARRIVE guidelines’ (Percie du Sert et. al 2020).
2.2.2 Category 2
2.2.2 Category 2. Forms of research with embryos, certain chimeras, and stem cell-based embryo models that are permissible only after review and approval through a specialized scientific and ethics review process. A comprehensive review should be coordinated with other relevant oversight, such as that provided by human subjects review committees, in vitro fertilization (IVF) clinic oversight bodies, and animal research review processes (see 2.2.1), and the research should comply with local law and policy. All such research should have a compelling scientific rationale and necessitate the use of these materials rather than employ alternative models. The research should use the minimum number of embryos necessary to achieve the scientific objective. Forms of research requiring comprehensive review by a specialized review process encompass the following activities:
Chimera research in which human pluripotent stem cells or their derivatives with broad potential are introduced into a) a non-human embryo or fetus in utero or b) a non-human embryo in vitro followed by transfer into a non-human uterus. Such experiments – if they are scientifically justified for the use of non-human primates above all other laboratory species – must exclude great and lesser ape species hosts (i.e., chimpanzees, gorillas, orangutans, bonobos, gibbons, and siamangs), as apes are prohibited from being used for invasive research in most parts of the world.
Human-Animal Chimeric Embryo Research
Recommendation 2.2.2.2: Chimeric embryo and in utero research described in ‘Category 2, i’ (see above) should proceed for the minimum time necessary to achieve the scientific aim. This research must proceed incrementally, stopping at well-defined timepoints to assess the degree and scope of chimerism during development before proceeding to full gestation, if full gestation is among the well-justified goals of the research. To avoid unpredictable and widespread chimerism, researchers should endeavor to use targeted chimerism strategies to limit chimerism to a particular organ system or region of the gestating chimeric animal.
Techniques such as blastocyst complementation, whereby a specific cell type or organ is effectively deleted as the host embryo develops, can lead to a specific cell type or organ being replaced entirely by derivatives from the donor-derived pluripotent stem cells. By itself this targeted chimerism may not prevent contributions elsewhere in the chimera, thus the need for an incremental approach. Nonetheless, if the host cells have an advantage over the donor cells, such as even a slightly faster rate of cell replication, then the donor cells will be disadvantaged and effectively selected against, leading to a little or no contribution outside the organ of choice.
As a general principle, non-human primate species should only be used when all other species, more distant in evolution from humans, are inadequate for the scientifically well justified research question being pursued. Appropriate research aims include understanding human development, understanding species barriers to chimerism, and treating disease. Any research involving non-human primates must utilize common laboratory species that are widely used in biomedical research (which excludes apes). Trained veterinary staff specializing in the care of non-human primates must be closely involved in the review and oversight of studies involving the transfer of human stem cells and their derivatives into nonhuman primate hosts.
2.2.3 Category 3
2.2.3B Category 3B: Prohibited research activities. Research under this category should not be pursued because of broad international consensus that such experiments lack a compelling scientific rationale or are widely considered to be unethical. Such research includes:
Research in which animal chimeras incorporating human cells with the potential to form human gametes are bred to each other.
Transfer of chimeric embryos mixing animal and human cells (whether predominantly animal or human) to the uterus of a human or great or lesser ape (i.e., chimpanzees, gorillas, orangutans, bonobos, gibbons, and siamangs).
Public Representation of Science
Recommendation 4.1: The stem cell research community should promote accurate, current, balanced, and responsive public representations of stem cell research.
The high level of public and media interest in the field provides stem cell scientists with ample opportunities to communicate their findings through a variety of popular and social media channels. The research community is encouraged to responsibly engage interactively with the public through outreach and communications and by providing opportunities for public comment and feedback on scientific advances.
While such opportunities may allow scientists to gain recognition and understanding for their work among non-specialists, they also have the potential to fuel inaccurate public perceptions about the current state of scientific progress, potential for application, and associated risks and uncertainties (Kamenova and Caulfield, 2015). Scientists, clinicians, bioethicists, science communications professionals at academic and research institutions, and industry spokespersons should strive to ensure that benefits, risks, and uncertainties of stem cell science are not understated, misrepresented or overstated (see Recommendation 3.3.4.1). Additionally, due to public interest and concern in the ethics of human pluripotent stem cell research, and in order to ensure complete transparency of research and translational activities, the origin of stem cell materials should be clearly specified in all communications.
Care should be exercised throughout the science communication process, including in the promotion of research and translation activities, as well as in the presentation of scientific results, the use of social media, and in any communication with print and broadcast media. Particular caution should be exercised when preparing press releases and other types of promotional material. Researchers should make efforts to seek timely corrections of inaccurate or misleading public representations of research projects, achievements, or goals. Scientists should also be particularly careful about disclosing research findings that have not passed peer review, as premature reporting can undermine public confidence if findings are subsequently disproven. For example, if researchers post online preprints that have not been peer-reviewed, readers should be informed of the preliminary nature of such manuscripts.
Researchers must unintentionally avoid and correct inaccurate misconceptions in any communications regarding chimeras, genome editing, and other issues with a long history in the public imagination. While organoids, chimeras, embryo models, and other stem cell-based models are useful research tools offering possibilities for further scientific progress, limitations on the current state of scientific knowledge and regulatory constraints must be clearly explained in any communications with the public or media. Suggestions that any of the current in vitro models can recapitulate an intact embryo, human sentience or integrated brain function are unfounded overstatements that should be avoided and contradicted with more precise characterizations of current understanding. This is particularly relevant to brain organoids and human-animal chimeras, where any statements implying human cognitive abilities, human consciousness or self-awareness, as well as phrases or graphical representations suggesting human-like cognitive abilities risks misleading the public and sowing doubts about the legitimate nature of such research. Likewise, forward-looking statements on inherently uncertain developments, such as predictions on time required until clinical application, the likelihood of product approval, or speculation on the potential economic impact of currently unrealized technologies, must be accurate, circumspect, and restrained.
The stem cell community should work closely with communications professionals at their institution to create information resources that are easy to understand without oversimplifying, and that do not underplay risks and uncertainties or exaggerate potential benefits. Similarly, research-sponsoring institutions and communications professionals have a responsibility to ensure that any informational materials referring to research achievements adhere to these principles. Additionally, the scientists in charge of the research findings that are featured in informational materials should review and agree to the content prior to release. For potentially sensitive or high-profile cases, it is advisable to seek additional comments from independent experts to ensure objectivity and balance, place research in context of existing body of evidence, and help identify study limitations and alternative interpretations of key findings.
-
This page assembles the sections of the Guidelines that specifically address research involving heritable genome editing. Other sections of the Guidelines may be relevant to such research (e.g., Section 2.1 Review Process, Section 2.3 Procurement and Informed Consent of Human Biological Materials, and Chapter 3. Clinical Translation of Stem Cell-based Interventions).
2.2.2 Category 2
2.2.2 Category 2. Forms of research with embryos, certain chimeras, and stem cell-based embryo models that are permissible only after review and approval through a specialized scientific and ethics review process. A comprehensive review should be coordinated with other relevant oversight, such as that provided by human subjects review committees, in vitro fertilization (IVF) clinic oversight bodies, and animal research review processes (see 2.2.1), and the research should comply with local law and policy. All such research should have a compelling scientific rationale and necessitate the use of these materials rather than employ alternative models. The research should use the minimum number of embryos necessary to achieve the scientific objective. Forms of research requiring comprehensive review by a specialized review process encompass the following activities:
Research involving the genetic alteration of human embryos or gametes used to make embryos in vitro.
2.2.3 Category 3
2.2.3A Category 3A. Research activities currently not permitted. Research under this category should not be pursued at this time because the approaches are currently unsafe or raise unresolved ethical issues. There may be valid reasons for undertaking the research in the future, but this should not proceed until the safety and ethical issues are resolved. Such research includes:
Research in which human embryos that have undergone modification to their nuclear genome are transferred into or gestated in a human uterus. Genome-modified human embryos include human embryos with engineered alterations to their nuclear DNA and embryos generated from a human gamete that has had its nuclear DNA modified, when such modifications could be inherited through the germline. While there are valid reasons for pursuing this line of research, which may include situations where correcting a deleterious gene variant is the only way that prospective parents may have a genetically-related child (National Academy of Medicine, National Academy of Sciences, and the Royal Society, 2020), conduct of such research will be dependent on appropriate policies, regulations, and oversight.
2.2.3B Category 3B: Prohibited research activities. Research under this category should not be pursued because of broad international consensus that such experiments lack a compelling scientific rationale or are widely considered to be unethical. Such research includes:
Research in which human embryos produced by reprogramming of nuclei are implanted into a human or animal uterus (often referred to as human reproductive cloning).
Emerging Categories of Embryo Research That Merit Close Review: Heritable Genome Editing
Recommendation 2.2.3.1: Until there is further scientific clarity regarding how to achieve desired genetic alterations, additional evidence for safety, and wider discussion and consensus on ethics (i.e., whether it should be done and, if so, under which circumstances), any attempt to edit the mitochondrial genome or modify the nuclear genome of human embryos for the purpose of human reproduction is premature and should not be permitted at this time (see Section 2.2.3A, Category 3A, a).
Preclinical research that entails modifying the nuclear genomes of gametes, zygotes, and human embryos may be permissible under a rigorous specialized oversight process (Category 2). Such research promises to enhance fundamental knowledge and is essential to inform deliberations about the potential safety and use of nuclear or mitochondrial DNA genome editing in strategies aimed at preventing the transmission of serious genetic disorders.
Scientists currently lack an adequate understanding of the fidelity and precision of techniques for genome editing of human embryos, as well as a full appreciation of the safety, ethics, and potential long-term risks and benefits to individuals born following such a process. This is described in more detail in the recent report, Heritable Human Genome Editing, from the International Commission on the Clinical Use of Human Genome Editing (National Academy of Medicine, National Academy of Sciences, and the Royal Society, 2020), which suggests a responsible translational pathway in certain circumstances, albeit one that cannot currently be met. Of note, the focus of this report was on developing a responsible translational pathway; it did not include a broad look at the societal and ethical issues, as these were outside its task. Such issues have been considered elsewhere (e.g. by the Nuffield Council on Bioethics). The forthcoming report from the WHO Advisory Committee on Developing Global Standards for Governance and Oversight of Human Genome Editing will bear in mind societal views and ethical principles, but this will focus on mechanisms of governance.
Basic and preclinical research is needed to minimize the potential harms resulting from intended and unintended edits, which could be passed to future generations, as well as direct or indirect effects of the editing process that could affect embryo viability or developmental potential.
3.4.8 Clinical Research that Involves Heritable Changes to the Human Genome
Heritable Genome Editing
Recommendation 3.4.8.3.1: Substantial preclinical research is needed to minimize the potential harm associated with clinical applications involving heritable genome editing; therefore, any attempt to modify the nuclear genome of human embryos for the purpose of reproduction is premature and should not be permitted at this time (see Section 2.1.3.3, Category 3A, a).
Any decision to proceed with heritable genome editing, where modified human embryos are transferred into a uterus or otherwise allowed to develop in utero, must be preceded with adequate preclinical research to minimize the potential harms from intended and unintended edits (see Recommendation 2.1.4). The first-in-human clinical uses should only be considered for the most favorable balance of potential harms and benefits and this will be most clearly defined for diseases and patients for which there are no viable alternatives. This may include prospective parents for whom there are no or very limited available alternatives for preventing transmission of diseases and conditions for which mortality is high and morbidity is severe. Other options for having a healthy child, including adoption, gamete or embryo donation, and preimplantation genetic testing, should be considered with appropriate counselling prior to any decision to proceed.
Recommendation 3.4.8.3.2: If the technical and safety challenges associated with human heritable editing are resolved (see Recommendations 2.1.4 and 3.4.8.3.1), any applications for the initial clinical use of human heritable genome editing should be evaluated on a case-by-case basis. This evaluation needs to consider not just the scientific methods, but also the societal and ethical issues associated with the proposed use.
The decision to proceed with first-in-human clinical uses needs to be taken openly with robust consideration of informed public opinion generated through meaningful public engagement. In addition, and critically, any experimental use of heritable human genome editing should only proceed in jurisdictions with appropriate and robust regulations and oversight.
A key consideration of potential uses of heritable genome editing is whether the prospective parents have feasible options for conceiving a genetically related child who does not inherit a serious genetic disease, such as preimplantation genetic testing and selection of embryos. The initial uses should be confined to prospective parents who lack reasonable alternatives.
It is important that the biological consequences of the intended genome edit are well understood, both for the immediate offspring and for future generations who might inherit it, in order to minimize the potential for an intended edit to have unintended deleterious consequences (on its own, via genetic interactions with other loci, or via environmental interactions). At present, the best way to achieve this goal is to use editing to change a known pathogenic genetic variant to one that is present in unaffected family members, common in the relevant population, or known not to be disease-causing.
Recommendation 3.4.8.3.3: A comprehensive regulatory and ethical framework for overseeing heritable genome editing must be established before any first-in-human clinical applications are considered. This framework should build on the existing regulatory frameworks for new biotechnologies, the practice of medicine, and the principles outlined in these guidelines (see Section 3.3 and 3.4).
The regulatory framework for heritable genome editing must ensure that there is robust multi-generational follow-up to identify adverse reactions that may occur due to inherited genome alterations. However, this needs to be done in such a way as to protect the confidentiality of the prospective parents and any children born. The framework must ensure that there is a robust informed consent process that builds on the informed consent process discussed in these guidelines (see recommendations 3.4.2.5 and 3.4.4.1) and includes a discussion of potential alternative treatments (if any) and the multigenerational risks and benefits of pregnancies involving the implantation of germline genome edited embryos, including those derived from genetically modified gametes.
Recommendation 3.4.8.3.4: Regulators, research funders, and academic and medical societies should seek to prevent the premature or unethical clinical uses of heritable genome editing unless and until the safety, ethical, and societal issues associated with the clinical use of heritable genome editing are resolved.
It is incumbent upon the entire biomedical research community to monitor for potential unethical and premature clinical uses of human heritable genome editing technologies. Researchers are strongly encouraged to report potential unethical uses to regulators, funders, licensing bodies, and academic societies to evaluate potential unethical uses of this technology.
-
This page assembles the sections of the Guidelines that specifically address research involving mitochondrial replacement techniques. Other sections of the Guidelines may be relevant to such research (e.g., Section 2.1 Review Process, Section 2.3 Procurement and Informed Consent of Human Biological Materials, and Chapter 3. Clinical Translation of Stem Cell-based Interventions).
2.2.2 Category 2
2.2.2 Category 2. Forms of research with embryos, certain chimeras, and stem cell-based embryo models that are permissible only after review and approval through a specialized scientific and ethics review process. A comprehensive review should be coordinated with other relevant oversight, such as that provided by human subjects review committees, in vitro fertilization (IVF) clinic oversight bodies, and animal research review processes (see 2.2.1), and the research should comply with local law and policy. All such research should have a compelling scientific rationale and necessitate the use of these materials rather than employ alternative models. The research should use the minimum number of embryos necessary to achieve the scientific objective. Forms of research requiring comprehensive review by a specialized review process encompass the following activities:
Transferring human embryos to a human uterus following mitochondrial replacement.
Mitochondrial Replacement Techniques
Recommendation 2.2.2.3: Further research should be undertaken to refine and assess the safety and efficacy of Mitochondrial Replacement Techniques (MRT), including minimizing a) the risk of mitochondrial carryover and b) disruptions to the interaction between mitochondrial and nuclear genomes. In addition, further research on polar body transfer techniques and the use of mitophagy or genome editing is needed to reduce or eliminate pathogenic mitochondrial DNA. Such research should be subject to review by a specialized oversight process as Category 2 Research (Section 2.1.5.2).
MRT is being explored to prevent the transmission of serious mitochondrial DNA-based diseases in at-risk pregnancies (see Section 3.4.8). MRT most commonly involves transferring the nuclear DNA from the prospective mother’s oocyte or fertilized oocyte (pronuclear stage) to that of a mitochondrial donor from which the nuclear DNA has been removed [maternal spindle transfer (MST) or pronuclear transfer (PNT), respectively]. The mitochondrial donor is selected to be free of known pathogenic mutations. Input from clinicians and scientists with relevant expertise in mitochondrial and embryo biology should augment the review process for evaluating clinical protocols that entail uterine transfer of human embryos for the purpose of human reproduction.
2.2.3 Category 3
2.2.3A Category 3A. Research activities currently not permitted. Research under this category should not be pursued at this time because the approaches are currently unsafe or raise unresolved ethical issues. There may be valid reasons for undertaking the research in the future, but this should not proceed until the safety and ethical issues are resolved. Such research includes:
Research in which human embryos that have undergone editing to their mitochondrial genome are transferred into or gestated in a human uterus, as current knowledge of such interventions is inadequate to ensure safety.
3.4.8 Clinical Research that Involves Heritable Changes to the Human Genome
Mitochondrial Replacement Techniques
Recommendation 3.4.8.1: Mitochondrial Replacement Techniques (MRT) should be offered only in the context of clinical investigation that is subject to strict regulatory oversight, limited to patients at high risk of transmitting serious mitochondrial DNA-based diseases to their offspring, when no other treatments are acceptable, and where long-term follow-up is feasible. International data sharing arising from initial uses is essential to help inform the field and ensure its appropriate use.
Initial applications of MRT should continue to be restricted to cases in which the probability of transmission of pathogenic mitochondrial DNA is very high, where preimplantation genetic testing is unlikely to identify embryos suitable for transfer, and where procedures are conducted in the context of clinical investigation that can contribute to generalizable knowledge about this currently unproven and experimental technique. Preclinical research in human embryo-derived stem cells following MRT indicated the possibility of levels of maternal mitochondrial DNA increasing with extended passaging, but the clinical relevance of these data is unclear. Concerns have also been expressed about the possibility of mito-nuclear interactions being disrupted by MRT, though these remain theoretical. Research on embryonic stem cells derived from embryos after MRT or on the embryos themselves maintained in vitro would help explore these issues. These experiments could only proceed in jurisdictions where the creation of embryos for research is allowed, and only where they have been permitted following review by a specialized oversight process (see Section 2.1).
Recommendation 3.4.8.2: There are inadequate clinical and preclinical data to justify the use of MRT to treat unexplained infertility associated with poor oocyte/embryo quality in women; therefore, it is recommended that this not be an intervention at this time.
MRT has been used in the clinic as a speculative treatment for infertility (Zhang et al 2016). Given the risks entailed and the absence of clear mechanisms and compelling rationale for the use of MRT for unexplained infertility, additional preclinical and clinical experience are required to establish safety and efficacy. In one reported pilot trial of MRT, embryonic development and pregnancy rates in patients of advanced maternal age did not increase (n= 30), and it was advised that such patients should not undergo MRT (Mazur, 2019). Data from another small (non-randomized) trial of MRT (n= 25), in women under 40 with previous multiple failures of IVF (Costa-Borges et al, 2020), suggest that further controlled trials and follow-up are required. Research conducted in vitro to understand the mechanism by which application of the techniques may help unexplained infertility (which might not involve mitochondria) should be conducted, notably because this may lead to alternatives that both circumvent the use of technically challenging methods and avoid any risks associated with heteroplasmy or disrupted mito-nuclear interactions.
-
This page assembles the sections of the Guidelines that specifically address research involving organoids. Other sections of the Guidelines may be relevant to such research (e.g., Section 2.3 Procurement and Informed Consent of Human Biological Materials).
2.2.1 Category 1
2.2.1A: Category 1A. Research determined to be exempt from a specialized scientific and ethics oversight process after being assessed by the appropriate existing mandates and committees for laboratory research. Category 1A research includes the following activities:
Research on stem cell culture systems that model specific stages of development or specific anatomic structures rather than the continuous development of an intact embryo or fetus. These would include but are not restricted to models of amnion formation, neural tube development, development of primordial germ cells, placental structures, 2D or 3D models of gastrulation or post-gastrulation events, and in vitro stem cell-derived organoids in culture that recapitulate most aspects of organ function, but not those that fall under subsequent categories.
Organoid Research
At this time, there is no biological evidence to suggest any issues of concern, such as consciousness or pain perception with organoids corresponding to CNS tissues, that would warrant review through the specialized oversight process. However, researchers should be aware of any ethical issues that may arise in the future as organoid models become more complex through long-term maturation or through the assembly of multiple organoids (Hyun et al. 2020).
Public Representation of Science
Recommendation 4.1: The stem cell research community should promote accurate, current, balanced, and responsive public representations of stem cell research.
The high level of public and media interest in the field provides stem cell scientists with ample opportunities to communicate their findings through a variety of popular and social media channels. The research community is encouraged to responsibly engage interactively with the public through outreach and communications and by providing opportunities for public comment and feedback on scientific advances.
While such opportunities may allow scientists to gain recognition and understanding for their work among non-specialists, they also have the potential to fuel inaccurate public perceptions about the current state of scientific progress, potential for application, and associated risks and uncertainties (Kamenova and Caulfield, 2015). Scientists, clinicians, bioethicists, science communications professionals at academic and research institutions, and industry spokespersons should strive to ensure that benefits, risks, and uncertainties of stem cell science are not understated, misrepresented or overstated (see Recommendation 3.3.4.1). Additionally, due to public interest and concern in the ethics of human pluripotent stem cell research, and in order to ensure complete transparency of research and translational activities, the origin of stem cell materials should be clearly specified in all communications.
Care should be exercised throughout the science communication process, including in the promotion of research and translation activities, as well as in the presentation of scientific results, the use of social media, and in any communication with print and broadcast media. Particular caution should be exercised when preparing press releases and other types of promotional material. Researchers should make efforts to seek timely corrections of inaccurate or misleading public representations of research projects, achievements, or goals. Scientists should also be particularly careful about disclosing research findings that have not passed peer review, as premature reporting can undermine public confidence if findings are subsequently disproven. For example, if researchers post online preprints that have not been peer-reviewed, readers should be informed of the preliminary nature of such manuscripts.
Researchers must unintentionally avoid and correct inaccurate misconceptions in any communications regarding chimeras, genome editing, and other issues with a long history in the public imagination. While organoids, chimeras, embryo models, and other stem cell-based models are useful research tools offering possibilities for further scientific progress, limitations on the current state of scientific knowledge and regulatory constraints must be clearly explained in any communications with the public or media. Suggestions that any of the current in vitro models can recapitulate an intact embryo, human sentience or integrated brain function are unfounded overstatements that should be avoided and contradicted with more precise characterizations of current understanding. This is particularly relevant to brain organoids and human-animal chimeras, where any statements implying human cognitive abilities, human consciousness or self-awareness, as well as phrases or graphical representations suggesting human-like cognitive abilities risks misleading the public and sowing doubts about the legitimate nature of such research. Likewise, forward-looking statements on inherently uncertain developments, such as predictions on time required until clinical application, the likelihood of product approval, or speculation on the potential economic impact of currently unrealized technologies, must be accurate, circumspect, and restrained.
The stem cell community should work closely with communications professionals at their institution to create information resources that are easy to understand without oversimplifying, and that do not underplay risks and uncertainties or exaggerate potential benefits. Similarly, research-sponsoring institutions and communications professionals have a responsibility to ensure that any informational materials referring to research achievements adhere to these principles. Additionally, the scientists in charge of the research findings that are featured in informational materials should review and agree to the content prior to release. For potentially sensitive or high-profile cases, it is advisable to seek additional comments from independent experts to ensure objectivity and balance, place research in context of existing body of evidence, and help identify study limitations and alternative interpretations of key findings.
-
Oversight
Recommendation 2.1.1: All research that (a) involves preimplantation stages of human development, in vitro human embryo culture, derivation of new embryo-derived cells or lines, integrated stem cell-based embryo models, or (b) entails the production of human gametes in vitro when such gametes are tested by fertilization or used for the creation of embryos, shall be subject to review, approval, and ongoing monitoring, as appropriate, through a specialized oversight process capable of evaluating the unique aspects of the science and the associated ethical issues (see below).
The specialized scientific and ethics oversight process encompasses the review of human embryo and related stem cell research. The process can be performed at the institutional, local, regional, national, or international level or by some coordinated combination of those elements and need not be served by a single, specific committee, so long as the oversight process as a whole occurs effectively, impartially, and rigorously. Provided appropriate expertise is available to ensure that the scientific, ethical, and legal aspects of the research can be rigorously evaluated, the specialized oversight can occur through preexisting institutional review processes that assess the participation of human subjects in research, the procurement of human tissues in and for research, or biosafety and ethical issues associated with research. For example, existing review bodies such as the Embryonic Stem Cell Research Oversight (ESCRO; Institute of Medicine and National Research Council, 2005), Stem Cell Research Oversight (SCRO; ISSCR Guidelines, 2006), or Embryo Research Oversight (EMRO; ISSCR Guidelines 2016) committees in the U.S., or the UK HFEA and regional ethics committees (RECs), are well positioned to perform review and oversight of embryo and related research. A single rather than redundant review is preferable as long as this is thorough and capable of addressing any uniquely sensitive elements of human embryo research and hESC research.
Recommendation 2.1.2: The specialized scientific and ethics oversight process must include an assessment of the scientific rationale and merit of research proposals, the relevant expertise of the researchers, and the ethical permissibility and justification for the research as discussed below.
Scientific rationale and merit of the proposal: Research involving human embryonic cells or human embryos and gametes requires that scientific goals and methods be scrutinized to ensure scientific rigor. Adequate and appropriate scientific justification for performing the research using the specified materials is required.
Relevant expertise of researchers: Appropriate expertise and training of the researchers to perform the stated experiments must be ascertained in order to ensure the appropriate use of research materials. For the derivation of new human embryo-derived cell lines, the formation of human embryo models from stem cells, or experiments that involve the use of human embryos, relevant expertise would include prior experience with embryo culture and stem cell derivation in animal systems and competence in the culture and maintenance of human embryonic stem cells. Researchers performing derivations of embryo-derived cell lines should have a detailed, documented plan for characterization, storage, banking, and distribution of new lines.
Ethical permissibility and justification: Research goals must be assessed within an ethical framework to ensure that research proceeds in a transparent and responsible manner. The project proposal should include a discussion of alternative methods and provide a rationale for performing the experiments in a human rather than animal model system, for the proposed methodology, and if the studies involve preimplantation human embryos, a justification for the anticipated numbers to be used.
Recommendation 2.1.3: The committee or body conducting the specialized scientific and ethics oversight process is responsible for (a) advising researchers on the categorization of research (see Recommendation 2.2), (b) determining whether a research proposal constitutes permissible or non-permissible research, (c) monitoring and periodically reviewing ongoing research, and (d) overseeing the provenance of the human pluripotent stem cell lines used in Category 2 Research (see section 2.2.2).
The responsible committee or entity should interpret these guidelines, define research practices, and monitor compliance. Researchers are encouraged to consult the committee or entity for advice on how to determine whether research is exempt as Category 1A (see 2.2.1)
Composition of Research Review and Oversight Bodies
Recommendation 2.1.4: The specialized scientific and ethics oversight process should be conducted by qualified scientists, ethicists, legal and regulatory experts, and community members who are not directly engaged in the research under consideration. The oversight process must include participants with the following perspectives:
Scientists and/or physicians with relevant expertise, including representation from scientists that are not directly engaged in the research under consideration. Relevant expertise includes areas of stem cell biology, assisted reproduction, developmental biology, and clinical medicine.
Ethicists with the ability to interpret the ethical justifications for, and implications of, the research under consideration.
Those familiar with relevant local policies and statutes governing the research.
Community members, unaffiliated with the institution where the research is conducted through employment, who are impartial and reasonably familiar with the views and needs of patients and patient communities who could be benefited by stem cell research, and community standards.
Additional members with relevant expertise not already represented on the oversight body should be included as required, for example to cover research involving human genetics, physiology, molecular biology, etc.
The policies and regulations of each country or jurisdiction will determine whether the specialized scientific and ethics oversight process will be performed by internal or external bodies at the institutional or national level. Participants in the specialized scientific and ethics oversight process should be selected based on their relevant area-specific expertise (e.g., scientific, clinical, ethics, research policy). Those engaged in the oversight process must be cognizant of potential financial and non-financial conflicts of interest that might compromise the integrity of the review. Such conflicts must be disclosed, evaluated, and minimized, or eliminated as much as possible.
-
2.3 Procurement and Informed Consent of Human Biological Materials
The procurement of human gametes, embryos, fetal tissues, and somatic cells is integral to the conduct of human embryo and stem cell research. Human biological materials must be procured in accordance with generally accepted principles of research ethics and laws and policies in their respective jurisdictions.
2.3.1 Review Process for the Procurement of Human Cells and Tissues
Recommendation 2.3.1. The review process for the procurement of human cells and tissues should be predicated on the source of the material and its intended use as described in the three tiers below.
Tier 1. Banked and historical cell lines. The procurement of cell lines from repositories or banks is permissible if the materials have been deposited and distributed consistent with the original consent for use of the donated human cells and tissues and these guidelines (see Section 2.4, Derivation, Banking and Distribution of Human Stem Cell Lines) and the standards at the time (Sugarman et al. 2008). Toward this end, the repositories or banks should require certification from depositors confirming the ethical provenance of such cells, including consent and ethics approvals. The use of historical cell lines from pathological specimens, such as HeLa, are permissible for use in stem cell research that is otherwise compliant with these guidelines. Likewise, stem cell lines procured from vendors are permissible for stem cell research, provided the vendor generated and distributed the stem cell lines in a manner consistent with the original donor consent and contemporaneous ethical and regulatory standards. The procurement of Tier 1 cell lines should not be used for reproductive purposes.
Tier 2. Fresh human somatic cells and tissues. The procurement of fresh human somatic cells and tissues for stem cell research purposes should be reviewed by existing research review committees bolstered by stem cell specific expertise in accordance with generally accepted principles of research ethics and laws and regulations in the respective jurisdiction and these guidelines (see Sections 2.3.2 and 2.3.3).
Tier 3. Gametes and embryos. The procurement of human gametes and embryos that are destined for use in human embryo research and stem cell research must be reviewed through the specialized oversight process and existing research review committees in accordance with generally accepted principles of research ethics and laws and regulations in the respective jurisdiction and these guidelines (see Sections 2.3.2 and 2.3.3).
Review by a specialized oversight process (Tier 3) or existing research review committee bolstered by stem cell-specific expertise must ensure that vulnerable populations are not exploited due to their dependent status or any compromised ability to offer voluntary consent and that there are no undue inducements or other undue influences for the provision of human cells and tissues.
2.3.2 Informed Consent for the Donation of Human Cells and Tissues
Recommendation 2.3.2.1: Embryos, fetal tissue, and other cells and tissues should be used in research only if voluntary informed consent was obtained from the donors before the research commences. The informed consent process should be robust and document the prospect of therapeutic and commercial applications as well as the potential research uses, such as the creation of hESCs, iPSCs, other immortalized cell lines, embryos, and gametes. In the case of fetal tissue, consent from the woman donating the tissue is sufficient. In the case of embryos made with donor gametes, this consent should be obtained from the gamete donors and the party(ies) with authorization to donate the embryo.
Most patients and research subjects may donate cells or tissues with broad consent to a range of future uses; however, the broad consent does not apply to use of donated cells and tissues for reproductive purposes. The consent may be obtained at the time of tissue collection or with a re-contact for additional consent to use donated cells and tissues for reproductive purposes.
In the case that human cells and tissues are procured from a minor or adult that lacks the decision-making capacity to provide informed consent, consent must be provided by a parent, legal guardian, or other legally authorized person. Whenever feasible, the assent of the minor or decisionally incapacitated adult is also strongly encouraged.
Empirical research has shown that informed consent is most effective as a dynamic, interactive, and evolving process as opposed to a static, one-time disclosure event (Flory and Emanuel, 2004). The informed consent document alone can never take the place of a meaningful dialogue between the person obtaining consent and the donors of human cells and tissues. The informed consent process can be enhanced in the following ways:
Whenever possible, the person conducting the informed consent dialogue should have no vested interest in the research protocol. If members of the research team participate in the informed consent process, their role and any other potential conflicts of interest must be disclosed, and care taken to ensure that information is provided in a transparent, accurate, unbiased manner.
The person conducting the informed consent process should provide ample opportunities for cell and tissue donors to ask questions and discuss their involvement in the research protocol.
Counseling services should be made available upon request to any potential providers of human cells and tissues prior to procurement.
Consent processes and documents should be revised in light of new research on informed consent for all types of human biological materials procurement and where relevant, ongoing studies of the long-term risks associated with oocyte retrieval.
Separating Research Consent from Treatment
Recommendation 2.3.2.2: Informed consent for research use must be distinct from informed consent for clinical treatment.
Decisions related to the provision of gametes or the creation of embryos for fertility treatment should be a voluntary choice that is free from undue influence by researchers who propose to use these cells in research. During the course of clinical treatment, researchers may not request that members of the fertility treatment team generate more embryos or harvest more oocytes than necessary for the patient’s optimal fertility treatment. Wherever possible, the treating infertility clinician should not be the investigator who is proposing to perform research on the procured materials.
Consistent with fetal tissue research guidelines issued by the Network of European CNS Transplantation and Restoration (NECTAR) and U.S. regulations, a woman’s decision to terminate a pregnancy must not be influenced by the possible research use of her fetus’ tissues (Boer, 1994; OHRP, 1993). Informed consent for fetal tissue procurement and research should be obtained from the woman only after her decision to legally terminate her pregnancy but before the abortion procedure, or after a spontaneous abortion. Medical procedures must not put the woman at any increased risk solely to facilitate the research use of donated fetal tissues. Clinicians obtaining informed consent and clinics at which informed consent is sought may not profit from the procurement of fetal tissues for research.
Review of Cell and Tissue Collection for Embryo and Stem Cell Research
Recommendation 2.3.2.3: Review of procurement protocols must ensure that cell and tissue donors are adequately informed about the specific aspects of their voluntary research participation.
Researchers should exercise care in seeking and obtaining informed consent from prospective donors. The informed consent process should take into account language barriers, the educational level and reading comprehension level of the research subjects, and any other impediments to good communication. Empirical research has shown that comprehension during the informed consent process improves with the use of interactive methods interaction (Flory and Emanuel, 2004). To facilitate the adoption of adequate and uniform standards of informed consent for the procurement of cells and tissues for research, the ISSCR provides template documents that can be downloaded and customized to specific protocols (Appendix 2). These sample documents will need to be customized for use in specific research studies and conform to local laws and policies.
If pluripotent stem cells are to be derived from procured cells or tissues, the informed consent document and discussion should cover information that addresses key aspects of human stem cell research, including but not limited to the fact that an immortal stem cell line could be established that is a partial or full genetic match to the cell or tissue donor and that the stem cell line could be shared with other researchers outside the institution and jurisdiction for other research purposes that may not be fully anticipated at this time. For a list of informed consent discussion points, see Appendix 3.
Incidental Findings
Recommendation 2.3.2.4: Researchers should develop a policy that states whether and how incidental findings will be provided to cell and tissue donors. This policy must be explained during the informed consent process. Cell and tissue donors should be able to choose whether they wish to receive incidental findings, if any. Reporting findings with relevance to public health may be required by law in certain jurisdictions.
During the course of research with human stem cell lines, particularly lines derived from somatic cells, investigators may discover information that may be of importance to cell and tissue donors, such as BRCA1/2 mutations. Because the net harms and benefits of disclosing incidental findings to cell and tissue donors are presently unclear, a single approach to managing incidental findings may not be appropriate across all studies and jurisdictions. When studies include a plan to disclose incidental findings to research subjects, researchers must offer a practical and adequately resourced feedback mechanism that involves donors’ physicians and, where possible, the verification of any discovered incidental findings.
For a given sample, secondary researchers should adhere to the incidental findings policies that were developed by the primary researchers (or others collecting cells and tissues) and disclosed to donors during the informed consent process.
If re-contact is required, instructions on how to report incidental findings (report to provider, researcher, institution, physician, etc.) should be specified in the material transfer agreement. Re-contact is a matter for primary research sites to manage. However, secondary researchers should be aware of the incidental findings policies of either of these responsible parties.
Successful implementation of a policy on incidental findings depends crucially on the traceability of cell line distribution. Therefore, all providers and recipients should ensure that cell lines are used under strict compliance with material transfer agreements and the regulations in the informed consent process.
Consent for De-identified Cells and Tissues
Recommendation 2.3.2.5: Researchers are encouraged to discuss the potential for genomic sequencing to connect de-identified cells and tissues to donors and their relatives during the informed consent process for the donation.
Cells and tissues donated for research are often de-identified to protect the privacy of donors. Due to advances in genomic sequencing, it may be possible for researchers to connect de-identified cell and tissue samples with donors or their relatives. Researchers are encouraged to require confidentiality when sharing genomic data that has the potential to connect donors and family members with de-identified cells and tissues.
2.3.3 Payments to Individuals Donating Cells and Tissue for Research
Recommendation 2.3.3.1: Research oversight committees must authorize all proposals to reimburse for out-of-pocket expenses to donors of embryos, sperm, or somatic cells.
Individuals who choose to provide previously stored cells and tissues for research should not be reimbursed for the costs of storage prior to the decision to participate in research. For the provision of fresh somatic cells or sperm for research, reimbursement for out-of-pocket expenses incurred by donors may be determined during the review process. For the provision of embryos or fetal tissue for research, no payment or valuable consideration of any kind beyond reimbursement of out-of-pocket expenses may be offered to donors for their procurement.
Recommendation 2.3.3.2: For the provision of oocytes for research, when oocytes are collected outside the course of clinical treatment, compensation for non-financial burdens should not constitute an undue inducement.
Because women carry particular burdens during the procurement of their gametes, their efforts should be acknowledged fairly and appropriately. At the same time, precaution is needed to avoid the potential for exploitation.
In jurisdictions where the provision of oocytes for research is legally permissible, the human subjects review committee and those responsible for conducting specialized research oversight must assess the safety and the voluntary and informed choice of women to provide oocytes for research according to the following standards:
There should be monitoring of recruitment practices of oocyte donors to ensure that the decision of women to donate their oocytes is free of undue inducement and exploitation.
In jurisdictions where research subjects are allowed compensation or valuable consideration for incurred non-financial burdens, the amount of financial recognition for the subject’s time, effort, and inconvenience must be reviewed to ensure that such compensation does not constitute an undue inducement.
Compensation for oocyte providers’ time, effort, and inconvenience, if permitted by local laws and human subjects review committees, should be reasonably consistent with compensation levels for other types of research participation involving similarly invasive and burdensome medical procedures. Compensation levels should aim to acknowledge oocyte providers’ non-financial burdens incurred as a result of their research participation, such as their physical discomfort and effort.
At no time should payments or other rewards of any kind be given for the number or quality of the oocytes that are to be provided for research.
Oocyte procurement must be performed only by medically qualified and experienced clinicians, and frequent monitoring and dose adjustment must be used to reduce the risk of ovarian hyperstimulation syndrome.
Due to the potential long-term effects of ovulation induction, women should undergo a limited number of hormonally induced ovarian stimulation cycles in a lifetime, regardless of whether they are induced for research or assisted reproduction. The limits should be determined by a thoughtful research review and oversight process, which should be informed by the latest available scientific information about the health risks.
A fertility clinic or other third party responsible for obtaining consent or collecting cells or tissues should not be paid for the material obtained. It should be eligible for specifically defined cost-based reimbursements and payments for professional services. Fertility clinics should not profit from providing tissues for research.
To help guide review committees through the ethical considerations surrounding oocyte collection and financial recognition of providers’ efforts, the ISSCR Ethics and Public Policy Committee developed an advisory report outlining their deliberations on these issues (Haimes et al., 2013).
-
This page assembles the sections of the Guidelines that specifically address the premature commercialization and unproven use of cellular products. Other sections of the Guidelines may be relevant to this issue (e.g., Chapter 4. Communications).
3.1 Classifying Stem Cell-, Cell-, and Tissue-based Interventions
Recommendation 3.1.1: Stem cells, cells, and tissues that are substantially manipulated or used in a non-homologous manner must be proven safe and effective for the intended use before being marketed to patients or incorporated into standard clinical care.
The therapeutic use of substantially manipulated stem cells, cells, or tissues or minimally manipulated stem cells, cells, or tissues for non-homologous treatments is complex, speculative, and has been shown to have risks to recipients. These products should be thoroughly tested in preclinical and clinical studies and evaluated by regulators as drugs, biologics, and advanced therapy medicinal products.
Minimally Manipulated Stem Cells, Cells, and Tissues
Minimally manipulated cells and tissues, such as, in some cases, fat tissue transferred from one part of the body to another, are generally subject to fewer regulatory requirements. When a stem cell-, cell-, or tissue-based intervention is claimed to be minimally manipulated and exempt from regulatory oversight on this basis, the responsibility rests on the clinician to invite independent scrutiny of their process of manipulation, such that scientific and regulatory experts can determine the proper level of regulatory oversight. When there is uncertainty or disagreement about the regulatory status of particular interventions, it is best to contact legally authorized regulatory bodies and seek their guidance concerning how specific interventions are classified. The US Food and Drug Administration, European Medicines Agency, Australian Therapeutic Goods Administration, Japanese Ministry of Health, Labour, and Welfare, and other regulators have released detailed standards to delineate when manipulation of cell-based products can no longer be considered minimal or their use homologous, and must therefore be subject to regulatory oversight as an advanced therapy product.
Substantially Manipulated Stem Cells, Cells, and Tissues
Substantially manipulated stem cells, cells, and tissues are subjected to processing steps that alter their original structural or biological characteristics. These processes can include isolation and purification processes, tissue culture and expansion of the cells, genetic manipulation, or other steps. For example, the extraction of cells from adipose tissue using enzymatic digestion, ultrasonic cavitation, or other means involves processing steps that can alter the original function of the cells imbedded in the tissue. The safety and efficacy profile of such an intervention needs to be determined for its particular indication using rigorous research methods. Safety and efficacy cannot be assumed because the composition of the intervention may differ from the original source tissue. Demonstration of safety and effectiveness will depend on the particular intervention and the specific condition targeted. Both to protect patients from risks and to help ensure that promising interventions are studied, it is critical that cells and tissues that have been substantially manipulated are evaluated by national regulators as drugs, biologics, and advanced therapy medicinal products.
Non-homologous Use of Stem Cells, Cells, and Tissues
Non-homologous use occurs when the stem cells, cells, or tissue are repurposed to perform a different basic function in the recipient than the cells or tissue originally performed prior to being removed, processed, and transplanted or otherwise delivered. For example, delivering adipose-derived stromal cells into the eye with the intent to treat macular degeneration would be a non-homologous use because the basic function of adipose tissue is not the trophic support of the retina. As with substantially manipulated cells and tissues, the non-homologous use of stem cells, cells, and tissues has potential benefits but can also pose serious risks. In the case of using adipose-derived stromal cells to treat macular degeneration, for example, there are well-documented reports of vision loss (Kuriyan et al., 2017). Such reports serve as a reminder that cells and tissues, depending on how they are administered, can cause serious harm. The benefit-risk ratio for non-homologous uses will depend on the particular intervention and the specific use. To protect patients from risks, and to ensure that necessary research is conducted, it is important that the safety and effectiveness of non-homologous uses be rigorously evaluated by regulators following the completion of well-designed and carefully controlled preclinical and clinical studies.
3.5 Unproven Stem Cell-based Interventions and Medical Innovation
The ISSCR condemns the administration of unproven stem cell- and other cell- and tissue-based interventions outside of the context of clinical research or medical innovation that is compliant with the guidelines in this document (see recommendation 3.5.2), particularly when it is performed as a business activity. Scientists and clinicians should not administer unproven interventions outside of clinical research or medical intervention as a matter of professional ethics. For the vast majority of medical conditions for which putative “stem cell therapies” or “regenerative therapies” are currently being marketed, there is insufficient evidence of safety and efficacy to justify routine or commercial use. Serious adverse events subsequent to such interventions have been reported and the long-term safety of most stem cell-, cord blood-, bone marrow-, and other cell-based interventions (i.e., mesenchymal stromal cells) remains undetermined. The premature commercialization of unproven stem cell interventions, and other cell-based interventions inaccurately marketed as “containing,” “acting on,” “derived from,” or “like” stem cells, not only puts patients at risk but also represents a serious threat to legitimate stem cell research. Widespread marketing and clinical use of unproven cell or tissue-based interventions reduces the number of individuals able to participate in credible clinical studies, risks jeopardizing the reputation of the field and causes widespread confusion about the actual state of scientific and clinical development.
Recommendation 3.5.1: The clinical use of unproven stem cell-based interventions should be limited to well-regulated clinical trials and medical innovations compliant with these guidelines (Recommendation 3.5.2) and local laws, policies, and regulations. Government authorities and professional organizations should establish and strictly enforce policies and regulations governing the commercial use of stem cell based medical interventions.
Historically, many medical innovations have been introduced into clinical practice without a formal clinical trials process. Some innovations have resulted in significant and long-lasting improvements in clinical care, while others have subsequently been demonstrated to be ineffective or harmful. Stem cell-based interventions typically entail complex manufacturing protocols that should rarely, if ever, be developed outside a formal clinical trials process. Nonetheless, in some very limited cases, clinicians may be justified in attempting medically innovative stem cell-based interventions in a small number of seriously ill patients. Although attempting medically innovative care is not research per se, it should not be embarked upon unilaterally. It is incumbent upon the clinician to obtain scrutiny by external experts through peer review, institutional oversight, and presentation of observations and data in peer-reviewed medical publication so that the knowledge can benefit all. Such limited attempts at medical innovation contrast with the advertisement, sale, and administration of unproven stem cell interventions.
Hospital Exemption
Regulators in some countries provide a “hospital exemption” to enable individualized care for patients. This exemption from requirements for regulatory evaluation of safety and effectiveness is only appropriate when the risks of the intervention are low and consistent with the risks typically associated with conventional surgical or medical procedures. Furthermore, the existence of such narrow exemptions should not be used as a vehicle for providing unapproved stem cell-based interventions or avoiding regulatory oversight, as occurs when cell-based interventions requiring pre-marketing authorization are inaccurately promoted as being exempt from regulatory scrutiny and approval requirements. Given the potentially serious risks associated with substantially manipulated tissues and cells and non-homologous uses, and the need to study their effectiveness, it is important that such interventions and uses be ineligible for these regulatory exemptions. In jurisdictions that provide hospital exemptions and have not established well-defined criteria that limit the scope of the exemption, regulators are urged to narrowly define them as including only low risk, minimally manipulated cells and tissues for homologous use.
Surgical Procedure Exemption
Regulators also often provide a narrow “same surgical procedure exemption,” excluding tissue- and cell-based interventions from certain regulatory requirements when cells or tissue are collected from, and delivered to, the same patient during the same procedure. These exemptions should be narrowly crafted to allow common surgical procedures like skin grafts, while excluding tissue and cell preparations that have been substantially manipulated or are being provided for a non-homologous use. This pathway should not be used to provide experimental and unapproved stem cell-based interventions.
Stem Cell Based Medical Innovation
Recommendation 3.5.2: Given the many uncertainties surrounding medical innovations involving stem cells and their direct derivatives, this pathway is rarely ethically and scientifically justifiable and should be limited to a very small number of patients and restricted to a) the off-label use of authorized therapies (see Recommendation 3.5.3), b) unproven interventions provided through expanded access pathways (see Recommendation 3.5.4), or c) minimally manipulated stem cell based interventions for homologous uses. Such interventions should only be provided to patients according to the highly restrictive provisions outlined in this section and the other referenced recommendations.
The written plan for the procedure must include:
Scientific rationale and justification explaining why the procedure has a reasonable chance of success, including any preclinical evidence of proof-of-principle for efficacy and safety.
Explanation of why the proposed stem cell-based intervention should be attempted rather than existing treatments.
Description of how the cells will be administered, including adjuvant drugs, agents, and surgical procedures.
Plan for clinical long-term follow-up and data collection to assess the effectiveness and adverse effects of the cell-based interventions.
The written plan is approved through a peer review process by appropriate experts who have no vested interest in the proposed procedure.
The written plan is approved by an independent oversight body after evaluating the risks and benefits for patients. In the academic context this would be routinely done through an institutional review process for human subjects research.
The patient is not eligible for an existing stem cell-based trial for this indication.
The clinical and administrative leadership of the healthcare institution supports the decision to attempt the medical innovation and the institution is held accountable for the innovative procedure.
All involved personnel have appropriate qualifications and training, and the institution where the procedure will be carried out has appropriate facilities and processes of peer review and clinical quality control monitoring.
Voluntary informed consent is provided by patients according to the ISSCR Informed Consent Standard (see Appendix 6).
There is an action plan for addressing adverse events that includes timely and adequate medical care and if necessary psychological support services.
Insurance coverage or other appropriate financial or medical resources are provided to patients to cover any adverse events arising from the intervention.
There is a commitment by clinician-scientists to use their experience with individual patients to contribute to generalizable knowledge. This includes:
Ascertaining outcomes in a systematic and objective manner
A plan for communicating outcomes, including negative outcomes and adverse events, to the scientific community to enable critical review (for example, as abstracts to professional meetings or publications in peer-reviewed journals). Initiating a formal clinical trial for the intervention in a timely manner after experience a very small number of patients.
Off-label Use
Recommendation 3.5.3 Off-label uses of stem cell-based interventions should be employed with particular care, given uncertainties often associated with off-label uses generally and associated with stem cell-based interventions specifically.
Physicians generally may use approved drugs and biologics for indications or patient populations other than those for which they have been shown to be safe and effective. This practice is commonly known as providing products on an “off-label” basis. Such off-label applications, distinct from administering products for the purposes for which they have been studied and approved, as specified on their prescribing information and package labels, constitute a common aspect of medical practice. Nevertheless, they present distinct challenges for stem cell, tissue or cell-based interventions.
First, depending on the jurisdiction, some stem cell-based interventions are not authorized for a specific use due to exemption from premarketing approval requirements. This can limit physicians’ access to reliable information on validated uses. Second, the complex biological properties of living cells and the limited clinical experience with cell-based therapies present uncertainties about long-term safety and effectiveness. Physicians should therefore exercise particular care when administering stem cell-based interventions on an off-label basis. As a rule, off-label use should only be offered when supported by high quality evidence or in situations consistent with current scientific knowledge, applicable regulations and institutional policies, and the standards of the international medical community. Patients must be informed in advance if a proposed off-label use has not been evaluated for safety and efficacy with respect to their specific medical condition. Off-label use of stem cell products is likely to increase as more stem cell therapies obtain pre-marketing authorization for particular indications. Providing such interventions on an off-label basis will need to be done with great caution, attentiveness to the available evidence base, and with the informed consent of potential recipients.
As a general principle, physicians should conduct controlled, supervised studies to establish safety and efficacy for new applications of products or interventions that have been approved in a distinct clinical setting. As evidence of safety and efficacy accumulates, regulatory bodies are provided with the data they require to consider expanding the indications that fall within the scope of product labeling.
Pre-approval Non-trial Access to Experimental Stem Cell-based Interventions
Recommendation 3.5.4 Pre-approval access to experimental stem cell-based interventions should be limited to well-regulated programs that require prior authorization from national regulators.
Patients understandably sometimes seek experimental interventions when there are no established and approved treatments for serious or terminal diseases and conditions. Regulatory authorization for pre-approval non-trial access programs (often described as “expanded access”) provides important checks and balances to ensure patient safety, facilitates drug development, and preserves the integrity of clinical trials. In particular, national regulatory bodies sometimes have access to important information about risks associated with particular investigational interventions that is not always available to individual patients or institutional review boards.
Substantial evidence to establish effectiveness for market approval
Recommendation 3.6.1.1 The introduction of novel products into routine clinical use should be dependent on the demonstration of substantial evidence of effectiveness in appropriately powered, well-controlled clinical trials, with statistically significant findings.
Regulatory approval for commercialization represents a key pivot point in a product’s translation. National governments and regulatory authorities should maintain rigorous review pathways to ensure that stem cell-based products conform to the highest standards of evidence-based medicine. Early interactions and advice during the product development process may support the accelerated development of safe and effective new therapies.
Even after clinical studies of the highest standard have demonstrated safety and efficacy and regulatory approval pathways have been cleared, close attention must be paid to ensuring the safety and effectiveness of interventions that have entered routine or commercial clinical use. Further, the fairness of access should be consistent with local legal requirements and standards and the standards of ethical, evidence-based medicine. These standards include ongoing monitoring of safety and outcomes and ensuring accessibility by those who have the most pressing clinical need.
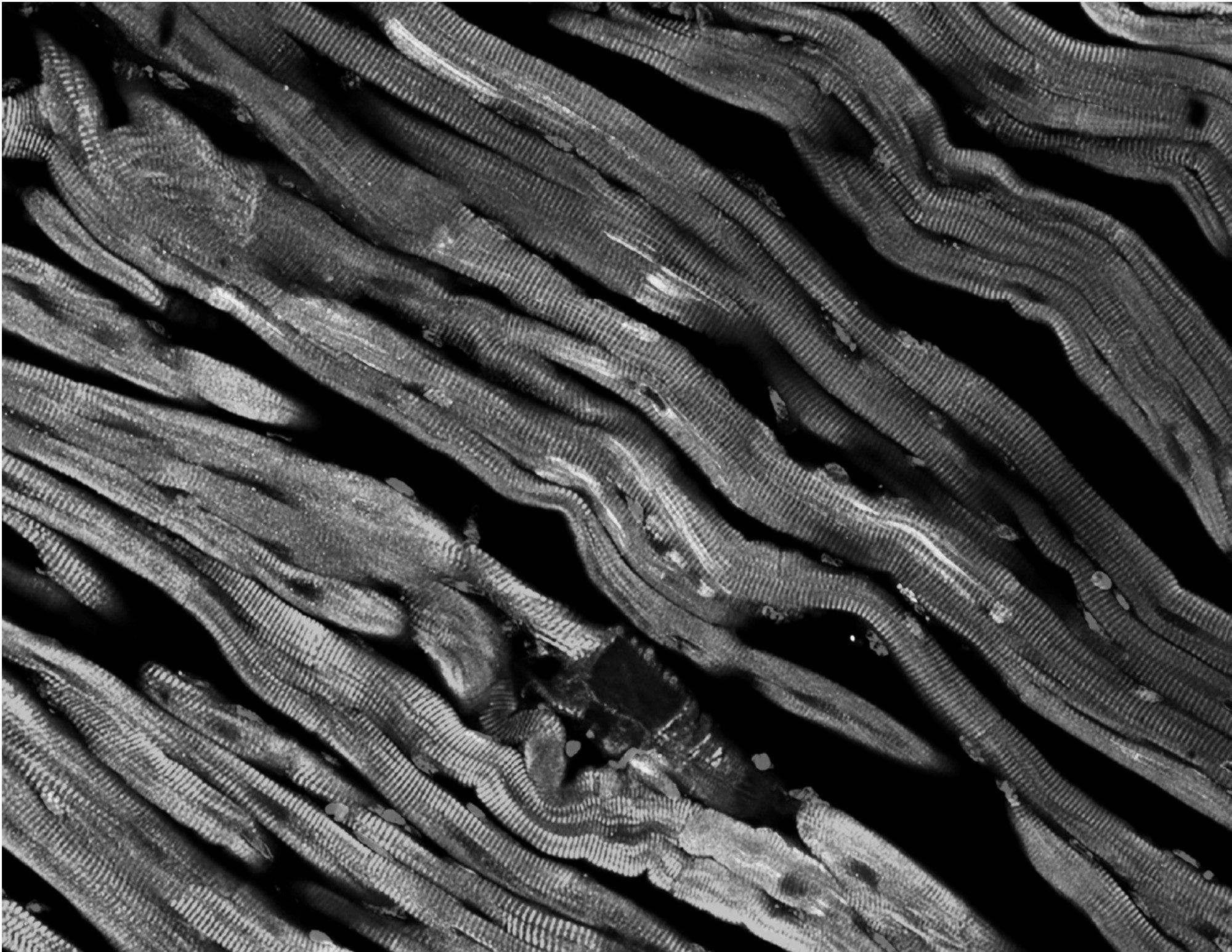
Retired Awards
The ISSCR Tobias Award Lecture was established in 2015 by the Tobias Foundation. The award recognized original and promising basic hematology research as well as direct translational or clinical research related to cell therapy in hematological disorders.
ISSCR Tobias Award Lecture (Retired 2021)
-
2021 Winner
Stuart H. Orkin, MD
Boston Children's Hospital, Dana-Farber Cancer Institute, and Harvard Medical School, USA2020 Winner
Margaret A. Goodell, PhD
Baylor College of Medicine, USA2019 Winner
Scott Armstrong, MD, PhD
Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, Harvard Medical School, USA
2018 Winner
Connie Eaves, PhD, FRS
Terry Fox Laboratory, BC Cancer Agency, Canada2017 Winner
John Dick, PhD, FRS
University Health Network of Canada/Ontario Institute for Cancer Research, Canada2016 Winner
Leonard I. Zon, MD
Boston Children’s Hospital, USA
The ISSCR Award for Innovation recognized a transformative breakthrough that has had a major impact on the field of stem cell research or regenerative medicine.
ISSCR Award for Innovation (Retired 2019)
-
2019 Winner
John Dick, PhD, FRS
Princess Margaret Cancer Centre, University Health Network, and Professor, University of Toronto, Canada2018 Co-Winners
Michele De Luca, MD, and Graziella Pellegrini, PhD
Center for Regenerative Medicine, University of Modena e Reggio Emilia, Italy2017 Winner*
Elaine Fuchs, PhD
The Rockefeller University/Howard Hughes Medical Institute, USA2016 Co-Winners*
Austin Smith, PhD, FRS, FRSE & Qi-Long Ying, PhD
Wellcome Trust Centre for Stem Cell Research, UK & University of Southern California, USA2015 Co-Winners*
Hans Clevers, MD, PhD, Irving Weissman, MD
Hubrecht Institute, The Netherlands Stanford School of Medicine, USA2014 Winner*
Azim Surani, PhD, CBE, FRS, FMedSci
Wellcome Trust/Cancer Research UK Gurdon Institute, UK2013 Winner*
James A. Thomson, PhD
University of Wisconsin, USA2012 Winner*
Rudolf Jaenisch, MD
Whitehead Institute for Biomedical Research/MIT, USA2011 Co-Winners*
Kazutoshi Takahashi, PhD & Shinya Yamanaka, MD, PhD
Center for iPS Cell Research and Application, Kyoto University, Japan*2011-2017 awards supported by the McEwen Centre for Regenerative Medicine
Previous Lawrence Goldstein Science Policy Fellows
2021-2024 Goldstein Policy Fellows
Brain Aguado, PhD
University of California, San Diego, USA
Justin Brumbaugh, PhD
University of Colorado, Boulder, USA
Tamra Lysaght, PhD
National University of Singapore, Singapore
2019-2021 Goldstein Policy Fellows
Mohamed Abou El-Enei, MD, PhD
MSPH Keck School of Medicine, University of Southern California, USA
Zubin Master, PhD
Mayo Clinic, USA
Kirstin Matthews, PhD,
Baker Institute for Public Policy, Rice University, USA
Established in 2019, the ISSCR fellowship program honors ISSCR member Lawrence Goldstein, PhD, for his longstanding commitment to policy and public service. Dr. Goldstein's advocacy before local, state, and national policy makers continues to make a significant impact on the field. The ISSCR’s policy fellowship program continues that legacy by training ISSCR members to become policy advocates.
Goldstein Science Policy Fellows serve a three year term, gaining firsthand policy and regulatory experience. They serve as ex-officio members of the Public Policy Committee, are invited attend advocacy days, take on self-directed special initiatives, have opportunities to speak in ISSCR programs, and receive mentorship from a member of the policy committee.
If you’re interested in joining the next cohort of policy fellows, please contact us.